Most people have experienced a problem with their eye at some point in their life. The most common conditions are sties, astigmatism, dry eye and conjunctivitis or pink eye. Each of these conditions are unique and have specific symptoms, causes, ways to avoid them and treatment methods. Dry eye and conjunctivitis, however, are often confused.
The Differences Between Dry Eye and Conjunctivitis
The table below highlights the main differences – and similarities – between these two conditions.
| Signs and Symptoms | Dry Eye | Allergic Conjunctivitis |
| Signs on the eye |
|
|
| Symptoms on the eye |
|
|
| Seasonal signs and symptoms | Can happen at any time | Most common during allergy seasons (spring/summer).Can happen at any time |
| Pattern | Worst at night and evenings | Worst in the morning and the evening |
| Common population groups affected |
|
Men under the age of 25. |
Let’s take a look at both conditions in greater detail.
Conjunctivitis
The so-called ‘pink eye’ happens when the conjunctiva is inflamed. The conjunctiva is the transparent film that covers the inside of the eyelid and most of the eyeball. When an irritation takes place at this point, the blood vessels start to swell, making the eye look pink. A number of causes are often at the heart of this, with the most common ones being:
- Bacteria, including STDs
- Viruses
- Irritants, including shampoos, chlorine and smoke
- Allergies, including pollen and dust
- Blocked tear ducts, which is most common in infants
- Having a foreign object in the eye
Conjunctivitis is a very annoying condition, but is usually not threatening, nor will it lead to permanent loss of vision. The only time it is considered a medical emergency is if it is related to an STD.
Most common symptoms of conjunctivitis include:
- Itchiness
- Redness
- Tearing
- Grittiness
- White, yellow or green discharge from the eye
- Crusting
- Blurry vision
- Burning
- Photophobia
Usually, if left untreated, conjunctivitis will solve itself. However, it is a very contagious condition, which is why it is important to receive proper medical care in order to prevent it from spreading. Treatment is usually very quick and effective by taking antibiotics, but individual patients must be seen to find the best treatment through them.
Treatment options, therefore, do vary, as the table below highlights.
| Cause of Conjunctivitis | Treatment |
| Bacteria | Antibiotics |
| Virus | Left to resolve itself. Close contact with other people must be avoided. |
| Irritants | Rinsing the eyes in order to remove the irritants. |
| Allergies | Identifying and removing the allergen is very important. This can be done through blood tests. You may want to see an allergist. |
The most important thing with conjunctivitis is to stop it from spreading any further. You must, therefore, frequently was your hands, avoid contact with others, use clean towels and linens. You must not touch your eyes, or share cosmetics and contact lenses.
Dry Eye
Dry eye syndrome is one of the most common eye problems in the world. It is believed that between 11% and 22% of the population suffers from it. Dry eye can happen due to a number of different reasons, although it tends to be because one of the components of tears is malfunctioning. In some cases, however, it is secondary to a different disease, such as HIV, lupus or rheumatoid arthritis. The condition tends to be more common in people over the age of 55 and those who wear contacts usually have the most severe symptoms.
Oftentimes, dry eye happens when one of the layers of the tear film (mucus, oil and water) is disrupted. This can happen for no discernible reason, or because someone suffers from Sjogren’s syndrome, for instance. Senile post-menopausal hyposecretion, taking systemic drugs (including diuretics and antihistamines), and long term contact lens use, can also cause it.
Many people find that the issue lies in the lipid layer of their tear film. This is produced by the Meibomian glands. When there is a lipid deficiency, tears evaporate too quickly, leaving the eye feeling dry. Many people who suffer from blepharitis, an inflammation of the eyelids, experience this. However, it can also happen with keratoconjunctivitis or other allergic reactions.
If the deficiency lies in the mucus layer, the problem is with the pathology of the goblet cells. This happens in people who suffer from some sort of chronic inflammation. Factors such as excessive use of heating or air conditioning, arid weather, dehydration and certain medications can make this worse.
Dry eye tends to be a chronic, persistent and very annoying condition. Some of the common symptoms include:
- Stringy mucus
- Stinging
- Blurry vision
- Photophobia
- Grittiness
- Excessive tearing
- Eye fatigue
- Irritation of the eye
- More allergic reactions
- Difficulty wearing contact lenses
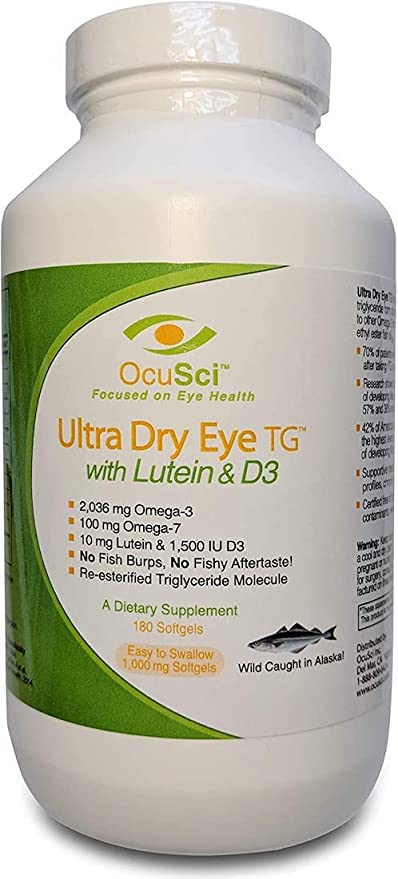
To find the best course of treatment, an ophthalmologist must first identify the cause of dry eye. Punctum plugs are often prescribed to people who suffer from dry eye syndrome as a result of anatomical abnormalities, post-surgical dry eye and low tear production. These can help to keep the eye moist. Alternatively, people can use eye drops, which are available over the counter. Supplementing with omega-3 is also found to be beneficial.
Dry Eye vs Conjunctivitis
It is very important to identify what is the real cause of your red eyes. This is why a medical professional will usually perform a physical examination, as well as ask you a number of questions. It is usually quite easy to determine whether or not the eye problem is caused by an allergy. If there is a family history of allergies, if you have experienced allergic reactions before, if you use eye drops to relieve your symptoms and if you ever use antihistamines, you are more likely to have an allergy. If, however, you find that your symptoms are worse when you watch TV, read a book or use a computer screen, or if certain climate conditions (dry air) make the condition worse, you are likely to suffer from dry eye.
Unfortunately, dry eye and conjunctivitis have a number of close similarities and this can make it more difficult to properly diagnose the condition. Medically, itching usually relates to allergies and burning relates to dry eye. However, the way patients describe the feeling can often be unclear. This is why doctors will also be on the lookout for tired eyes, grittiness and dryness complaints, which is more common in dry eye syndrome. If, however, patients say that their eyes are puffy, their lids are swollen, their eyes are always at ‘half-mast’ or that they experience a feeling of having hot, tight eyes, then it is more likely to be an allergy.
Some doctors will ask patients what happens when they rub their eyes. In case of an allergy, rubbing will usually make it worse, whereas it will improve the condition with dry eye. However, because it is so important for people not to rub their eyes, most doctors will not actually use this test.
Tearing is common in both conjunctivitis and dry eye, so the presence of tears does not conclusively point to a condition. Generally, people with dry eye tear less, noticing it more during the evening or when they are tired. In case of an allergy, tearing is usually constant. Hence, tearing is an important investigative tool, but one that isn’t completely fool-proof.
Similarly, eyelid crusting can be indicative of either. If the skin around the lids becomes flaky and there are seborrheic signs like collarettes, it usually points to blepharitis and dry eye. If, however, excessive mucus is present, it is more likely to be an allergy. Additionally, acute allergic reactions can cause the eyelids to swell up significantly.
Finally, most people with dry eye syndrome will also experience dryness elsewhere. This includes the mouth, nose and reproductive organs. People with allergies, by contrast, usually experience congestion of some sort, leaving the throat to feel sore and itchy.
Having Them Bot
It is also possible for someone to suffer from both dry eye and conjunctivitis. In this case, finding the most effective treatment is usually down to treating the most annoying symptom. A lubricating agent with anti-allergens is often recommended. While antihistamines are known to cause dry eye, specific ocular antihistamines do not. In fact, some of these (such as olopatadine) were actually shown to improve the symptoms of dry eye. Generally, however, people will be asked to also use a tear substitute, which is available over the counter. It is very important, however, to choose one that is free from preservatives.
Other common medications offered to people who suffer from both conjunctivitis and dry eye syndrome include:
- Systane PF
- Restatis
- Doxycycline
- Corticosteroids
Resources and References:
Facts About Dry Eye – General information on dry eye. (National Eye Institute)
Allergic Conjunctivitis and Dry Eye Syndrome – Comparing dry eye and allergic conjunctivitis. (NIH.gov)
Conjunctivochalsis vs. Dry Eye: Do You Know the Difference? – Differences between dry eye and conjunctivochalsis. (Ophthalmology Management)