Glaucoma happens when the eye is no longer able to properly balance the amount of tears that are produced, and the amount that dries away. The main cause of this, in turn, is that the internal fluid pressure of the eyeball is out of balance. Once it rises dangerously high, glaucoma happens. The eye is different from a balloon, however, as it cannot simply deflate slightly. Rather, the pressure continues to build up until the nerve fibers of the optic nerve are damaged beyond repair, leading eventually to vision loss.
The Anatomy of the Eye
During the progression of glaucoma, eye neurons start to become damaged. This leads, at first, to loss of peripheral vision. However, the damage also affects the brain. In fact, this is where it happens first, as the brain is no longer able to make the connections with the eye. This was discovered by researchers at Vanderbilt University in 2010. This may mean that a whole new approach to glaucoma treatment could also be developed.
To understand glaucoma, you must also understand how fluid moves in the human eye:
- The ciliary body produces the eye’s clear fluid. This body is behind the iris.
- The fluid is called aqueous humor, filling the space between the front of the iris and the back of the clear cornea.
- The drainage angle enables the fluid to exit the eye.
- Through the angle, the fluid filters into the white part of the eye, joining its veins.
If there is a disruption in this flow, eye pressure can increase.
There are different types of glaucoma, as the table below highlights.
| Type of Glaucoma | Details |
| Open angle glaucoma (OAG) |
|
| Angle closure |
|
| Low tension |
|
| Exfoliation syndrome |
|
| Pigmentary |
|
It is also possible for glaucoma to be caused to an eye injury, tumor or disease. Very rarely, children are born with glaucoma.
There are a number of risk factors to also be aware of. Simply having high pressure in the eye doesn’t necessarily mean that glaucoma is present. However, this is the biggest risk factor of all. Other risk factors include:
- Your age
- Your ethnicity (African ethnicities are most at risk)
- Having a family history of glaucoma
- Having a thin cornea
- Being nearsighted
- Having sustained eye injuries
- Having used steroids (illegal and prescription)
- Having experienced shock or severe anemia
A number of studies have taken place at the University of Michigan’s Kellogg Eye Center and they found that people with hypertension and/or diabetes may be at an increased risk of developing OAG. It is important to have regular eye examinations by a licensed ophthalmologist, as they will be able to determine whether you need to receive treatment, whether you have to be monitored, or whether you do not seem to be developing glaucoma.
Glaucoma and Dry Eye
The vast majority of patients with glaucoma also have dry eye. In many cases, patients experience dry eye syndrome (DES) symptoms, but do not know that this is the condition they have. This is particularly true because people with glaucoma and dry eye often have excessive tearing. Alternatively, they feel like there is something in their eye, leading to them thinking there is actually a foreign body somewhere in the eye.
Each person experiences DES differently. For many people, the symptoms go in remission for long periods of time, and they can also be very subtle. However, that doesn’t make them any less annoying and treatment should be provided to increase someone’s quality of life.
As people age, DES becomes more common, just as glaucoma does. It is believed, from studies, that some 40% to 50% of people who have been diagnosed with glaucoma also have DES. Women are particularly at risk of having both conditions at the same time.
It can be difficult for patients and doctors alike to find an appropriate treatment. In terms of comfort, treating DES is perhaps the most important thing of all, as well as in terms of keeping the surface of the eye as healthy as possible for as long as possible. Glaucoma can lead to complete loss of vision, however, which is why patients with both glaucoma and DES will be treated for glaucoma first. This is despite the fact that DES will bother the patient more.
DES can be caused by a range of different things, not all of which are directly linked to glaucoma. Because the eye is such a delicate part of the body, it is all too easy for something to go wrong. For instance, the eyelids or their Meibomian glands can become inflamed. People may have had eye surgery or a type of eye infection. They may also live in arid regions or over-use their heating and air conditioning. Interestingly, prolonged use of glaucoma drops also leads to dry eye syndrome.
Treating Glaucoma and Dry Eye
It is usually best to provide patients with a combination of treatments. This does mean, however, that most people will have to try and test a range of different drops and medications before they find the combination that is right for them. For dry eye, patients will usually be prescribed:
- Eye drops, also known as artificial tears
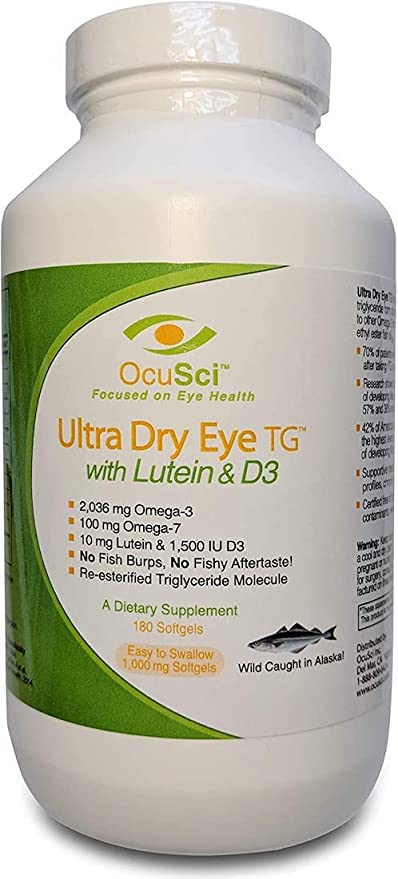
- Vitamins and supplements with cardiovascular benefits, including omega-3 and fish oil clinically work well
- Cyclosporine, usually as a drop, which helps to suppress any inflammation in the eye
- Warm compresses or eyelid scrubs, which also help to bring down inflammation
- Other anti-inflammatory medication such as doxycycline
Both dry eye syndrome and glaucoma are chronic and both require treatment. In most cases, eye drops will be required and it is known that patients often find it difficult to properly complete the treatment they need. It is vital, however, that the surface of the eye remains as healthy as possible not just in terms of patient comfort, but also to help increase the chances of glaucoma surgery being successful.
The patient and the doctor have to work together in order to find the best possible treatment for both dry eye and glaucoma. In many cases, the eye drops used for glaucoma make DES worse – or cause it – and the symptoms often significantly lower the patient’s quality of life. A new study suggests that this is even more common in people of African ethnicity.
The study completed Miami, FL’s Bascom Palmer Eye Institute demonstrated that there is a very clear link between race and how glaucoma medication affected dry eye, which in turn affected quality of life. Patients of African ethnicity noticed that their quality of life was significantly more affected compared to Caucasian patients taking the exact same medication.
In the study, just short of 500 patients at a Miami veterans’ health clinic were asked to complete the DEQ5 (Dry Eye Questionnaire 5) and the IDEEL (Impact of Dry Eye on Everyday Life). This enabled researchers to measure the impact DES had on the quality of life of patients. 353 of the participants had glaucoma and were currently receiving treatment through eye drops. A further 114 patients were the control group, who did not have a history of any type of eye disease or problem. Out of the 353 patients, 60% were of African ethnicity and 39% were Caucasian.
The study showed that, while it is clear that glaucoma eye drops are vital to stop the condition from getting worse, they can also make the symptoms of dry eye worse at the same time. It was noted that 34% of patients who used eye drops experienced dry eye symptoms, compared to just 25% in the control group. The more drops were used, the more severe the symptoms became as well. As such:
- 25% of people who did not use drops experienced DES
- 27% of people who used one or two drops experienced DES
- 40% of people who used three drops or more experienced DES
It was also found that the patients who did receive treatment for glaucoma through drops were also more likely to experience lower emotional well-being. However, there was no link between drops and ability to perform daily tasks. It was in this part of the study, however, that the racial disparity became most pronounced.
While there was no surprise in the fact that the more drops people used, the worse their DES symptoms would get, the fact that those of African ethnicity suffered more was surprising. As a result, it is now recommended that ophthalmologists take into consideration the ethnicity of their patients, thereby making sure that those of African ethnicity in particular are queried about the adverse effects they are experiencing. It may be that surgery or laser trabeculoplasty is more suitable for them. Quality of life of patients is incredibly important, after all, and must be considered.
Resources and References:
- Glaucoma and Dry Eye: Principles and Parallels – Connection between dry eye and glaucoma. (Rewiew of Optometry)
- Glaucoma and Dry Eye: A Tough Combo – Dry eyes and glaucoma. (Review of Ophthalmology)
- Study Focuses on Relationship Between Glaucoma and Diabetes, Hypertension – How glaucoma, hypertension and diabetes are interrelated. (Kellogg Eye Center)
- Dry Eye Syndrome-Related Quality of Life in Glaucoma Patients – Dry eyes in glaucoma patients. (NIH.gov)