On both your upper and lower eyelids, you will find Meibomian glands near your lashes. Whenever you blink, the pressure makes these glands to excrete oil. This oil, in turn, ensures tears do not evaporate too quickly, allowing them to keep the eye moisturized. Some people, however, have Meibomian gland dysfunction (MGD), which means that the glands produce either too much or, more commonly, too little oil.
What Is Meibomian Gland Dysfunction?
There are a few different types of MGD, but the most common one is posterior blepharitis. When you first develop this, it is unlikely that you will notice any symptoms. However, if not treated, MGD can make the eyelids inflamed, and it can also lead to dry eye syndrome (DES). MGD happens for a range of reasons although most often the glands are blocked because secretions become too thick. If the glands become chronically blocked, they will be unable to secrete oil. This leads to permanent dry eye syndrome due to changes in the tear film.
Essentially, your eyes are on strike. A tear is made up of three essential elements, which are the aqueous layer (water), the mucus layer and the lipid (oily) layer. In MGD, the oily layer becomes disrupted, leading to DES. Usually, a Tear Break-Up Test (TBUT) is able to measure whether or not you have MGD.
MGD is often undiagnosed because the symptoms are not noticeable until the condition becomes chronic. If it is diagnosed before then, it is often not properly treated. While most MGD is caused by blepharitis (inflammation), it can also be atrophic.
Causes of MGD
The exact causes of MGD are often not known. However, a number of risk factors seem to be present, including:
- Age, with MGD being more common in older people.
- Taking prescription medication, particularly retinoic acid (acne treatment), HRT (hormone replacement therapy for menopausal women), antidepressants, antihistamines, anti-androgen medication (used to treat prostatic hypertrophy).
- Having an endocrine disorder, like being pregnant or going through menopause.
- Wearing contact lenses for too long (either keeping them physically in for too long or wearing them for many years).
- Immune system disorders such as acne and atopic rosacea, psoriasis, rheumatoid arthritis and Sjogren’s syndrome.
Diagnosing MGD
By looking at how the edges of the eyelids appear and what the composition of the oily substance of the Meibomian glands is, a doctor can diagnose the type of MGD that is present. Most commonly, it is a latent type of MGD, which causes then dry eye symptoms, but no other changes to the eyelids. Most people will experience excessive weeping at night, which is noticeable when they wake up the next morning. Some also complain about irritation. The symptoms often get worse in environments with excessive heating or air conditioning, or when people use computer screens for a long time. If MGD is recognized and properly treated, it can help to avoid chronic dry eye syndrome from developing as well. While MGD is caused by changes in the Meibomian glands, these changes do not have to be permanent if proper treatment is provided.
Dry Eye or MGD?
It is quite common for people to confuse MGD and dry eye syndrome. However, technically, dry eye syndrome happens when there is a deficiency in the aqueous layer of the tear film. This can be treated with artificial tears, ointments or punctal plugs. Interestingly, however, many cases of dry eye are actually caused by MGD. In fact, ophthalmologists believe that as much as 70% of cases of DES are actually MGD. Most people who have DES, or who believe they have DES, will purchase over the counter eye drops to make this better. These eye drops often contain preservatives. Long term use of these drops can actually make DES worse. If the DES is actually caused by MGD, eye drops with preservatives will almost always make the condition worse, so should be avoided.
Blepharitis or MGD?
Everything in the eye is related. People who have blepharitis (inflammation of the eyelid) will inevitably develop MGD and this, in turn, will cause DES. However, blepharitis is not the same as MGD. In fact, it is possible for someone to heal from blepharitis, while continuing to have MGD. Symptoms of blepharitis include:
- A burning sensation in the eyes
- Dryness of the eyes
- Stickiness
- Itching
- Photophobia (light sensitivity)
- Excessive watering of the eyes
- Feeling like there is a foreign body in the eye
- Sty or chalazion
- Blurry vision that seems to come and go
Recognizing MGD
The symptoms of MGD, blepharitis and DES are all very closely related. This is why it is so important to seek medical advice, so that the proper treatment can also be found. Most people with MGD will have any or all of the following symptoms:
- Tearing
- A burning sensation
- Feeling like a foreign body is in the eye
As previously stated, the TBUT test can determine whether MGD is actually present or not. Unfortunately, many doctors will only examine the eyelid region, where they are likely to notice the presence of blepharitis. If the blepharitis becomes worse, it may be very difficult to express from the Meibomian glands, which means it does have to be treated first.
List of MGD Treatment Options
The table below highlights some of the common treatment options for MGD.
| Treatment Option | Details |
| Warm compress | When the eyelids are heated, they will automatically start to produce more oil. This will then get rid of any oil in the glands that has solidified and caused a blockage. Leaving a washcloth in place for two minutes should be long enough to allow oil to flow freely again. |
| Massage | By gently applying pressure with either the fingers or a Q-tip to the margin of the lids, next the lash line, may help. However, you must be sure that your fingers or the Q-tip are properly sterile, or eye infection may follow.
To massage, you must look up and gently roll your finger on the lower lid upwards and then look down and roll your finger on the upper lid downwards. Do not do this more than twice per day. Once is preferred, as you can actually make any irritation worse. |
| Lid scrubs | A lid scrub helps to get rid of debris, bacteria and oil, while at the same time stimulating oil production. You can rub along the lid line with a washcloth on both the upper and lower lid. |
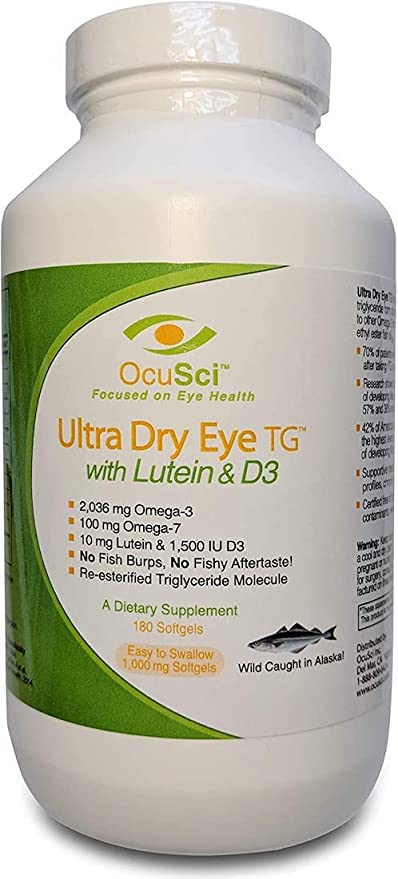
| Flax seed oil | Some people have noticed that by adding omega-3 fats to their diet, they experience fewer problems with MGD. This can be taken as a supplement, or directly by adding it to cereals and juices, for instance. You should not take flax seed oil if you also take blood sugar lowering medication or blood thinning medication. Other omega-3 supplements may also be beneficial. |
| Antibiotics | If your MGD has turned into an infected blepharitis and is caused by bacteria, then an oral or topical antibiotic may be beneficial. |
| Lifestyle changes |
|
Resources and References:
- Treating Dysfunctional Meibomian Glands – Treatment of Meibomian gland diseases. (Review of Ophthalmology)
- The Experts Open Up on Meibomian Dysfunction – Information on Meibomian gland problems. (Review of Ophthalmology)
- Put the Squeeze on Meibomian Gland Disease – Treatment of Meibomian gland disease. (Review of Optometry)